Comparing Healthcare Models and their Role in the COVID-19 Response
COVID-19 has challenged healthcare systems in every country and shed light on some of the flaws in their frameworks. Lessons can be learned from this situation to improve how care is delivered generally and during emergencies. It can be overwhelming to tune into a discussion about healthcare and the complex policies and options centered around its reform, but this information can be broken down to its fundamentals. As the presidential election in the United States draws closer, it is important to become more informed about the different modes of healthcare administration.
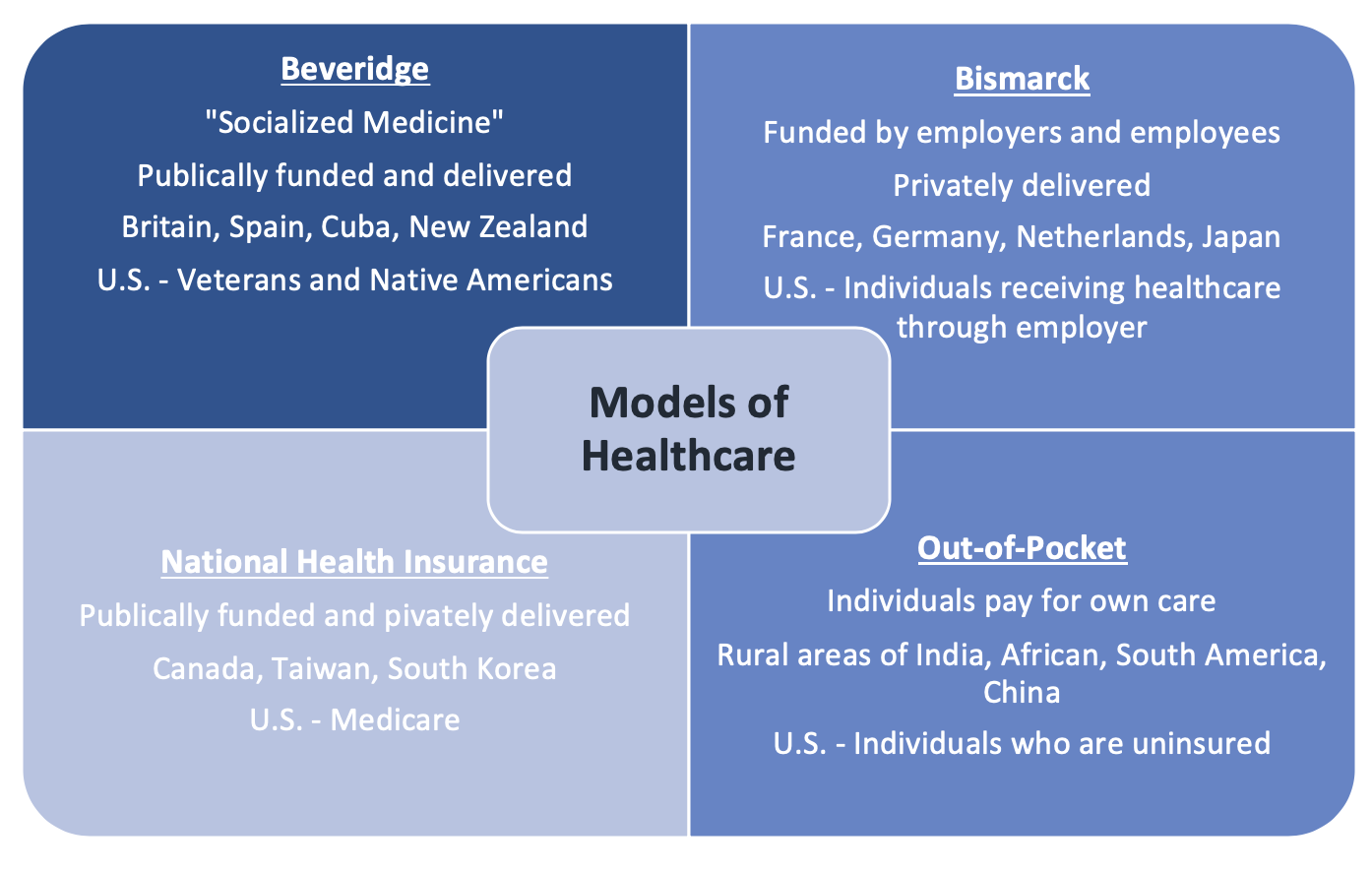
The Four Models of Healthcare
The healthcare systems of different countries are based off four models:
Beveridge
Bismarck
National Health Insurance
Out-of-Pocket
Often times, it is not one or the other, but a blend that is employed in most countries.
Beveridge Model
The Beveridge model is known as “socialized medicine” because all citizens of a country will have healthcare that is financed by their government using tax payments. Since the government owns hospitals and other medical centers, most physicians are considered government employees. Healthcare costs are also low because the government is the sole payer, which eliminates market competition. The idea behind this system is that healthcare is a human right and citizens are guaranteed universal coverage. Because patients contribute through taxes, they do not have to pay anything out of pocket after medical services.
Additionally, a disadvantage of a system that provides equal access to everyone is long waiting lists and over-use that can lead to higher costs. In times of a crisis, a decrease in public revenue can lead to a decrease in funding for services while patient numbers increase, causing a burden on the system. This model was developed in the United Kingdom and has spread to Northern Europe and other countries such as Spain, New Zealand, and Cuba.
Bismarck Model
In the Bismarck model, an insurance system is funded by both employers and employees as deductions are made from payroll to form a sickness fund. Profit is not made from this and the insurance covers every citizen regardless of preexisting conditions. Unlike the Beveridge model, this model has private physicians and hospitals instead of government owned hospitals. Furthermore, there is a shift as healthcare is considered a privilege instead of a right because it benefits individuals who can financially contribute to their own care. This results in concerns about how to provide care for people unable to work or unable to afford the payments.
Countries that use the Bismarck model also have differences in their insurance systems. For example, France has a single insurer while Germany has competing insurers and Japan has non-competing insurers.
National Health Insurance Model
The National Health Insurance model blends together aspects from both the Beveridge and Bismarck models. Government run insurance programs collect a premium or tax from citizens which is comparable to the Beveridge model. However, the providers are from a private sector which resembles the Bismarck model. This type of universal insurance is less expensive because profit is not made and claims are not denied, allowing patients to choose their providers. Because everyone is covered regardless of income level, costs are controlled by limiting the types of services paid for and having waiting lists. The waiting lists for services such as hip replacements for the elderly and neurosurgery appointments can be very long and this is often seen as a significant health policy issue. Countries that use this type of insurance system and face these issues are Canada, Taiwan, and South Korea.
Out-of-Pocket Model
The Out-of-Pocket model is common in less developed nations that do not have the resources to organize a national healthcare system. Patients pay for the cost of their treatment or procedure out-of-pocket. The unfortunate result is that the wealthy get treated while the poor either remain sick or die. This is seen in rural South America, India, Africa, and China.
The United States incorporates all of these models to form a patchwork. Veterans in America are treated using the Beveridge model where the government finances care. The eldery over 65 have Medicare like the National Health Insurance model while working Americans have insurance funded by employees and employers as seen in the Bismarck model. Healthcare disparities in impoverished neighborhoods are observed where people are either underinsured or uninsured, which corresponds to the Out-of-Pocket model.
How Different Countries Responded to COVID-19
The United Kingdom (Beveridge model), in which healthcare is completely financed by the government, had a delayed effort in dealing with COVID-19. Lockdowns and closures came weeks after other European nations. The National Health Service (NHS) planned to buy space in private hospitals as well as postpone non-emergency procedures to free up hospital beds. The government also formed makeshift hospitals from various buildings and retrained and redeployed former health care workers and specialists. Problems pertaining to lack of ventilators and personal protective equipment (PPE) were solved by importing, accepting loans from the army, and encouraging manufacturing companies to produce them.
Citizens in South Korea, which employs the Bismarck model, have services delivered through the private sector. They had a quicker response to COVID-19 due to experience dealing with the Middle East Respiratory Syndrome (MERS) outbreak in 2015. South Korea was prepared for a healthcare emergency and designated a health crisis coordinator. Just after the first case in January, diagnostic tests were developed and drive-through testing sites were established. Testing was free with costs being covered by the health insurance public corporation and both the central and local governments. Additionally, COVID-19 hospitals were set up where solely patients with the virus were treated while other patients visited non-COVID-19 hospitals. The private sector aided these efforts by producing medical supplies for the public to use.
Taiwan, with its National Health Insurance Model, provides its residents benefits which are financed by payroll taxes and taxes on products such as tobacco and the lottery. Taiwan had an epidemic response plan established due to lessons learned from the Severe Acute Respiratory Syndrome (SARS) outbreak in 2003. Testing was conducted early on and for free. Phone applications were used to track individuals’ data while body-heat sensors were used to detect body temperature, determine close contact to patients with the virus, and impose quarantines. The government employed a useful tactic by tracking patients who had severe respiratory symptoms and had also tested negative for the flu. They were then retested for COVID-19 which was helpful in preventing spread.
India, which has an Out-of-Pocket model, is facing many challenges in its COVID-19 Response. To begin with, India has some of the lowest testing rates with 1,832 tests conducted per 100,000 individuals. The rural, low-income areas are seeing low testing rates as well as high infection rates and receiving little help from the government. The health care system is poor in its emergency preparedness, health care access, and countermeasures. Quarantine centers are usually overcrowded and unhealthy, and other medical facilities have low capacities.
The United States, with a blend of all the models of healthcare, had a disjointed COVID-19 response. Some of the initial issues were failure to both implement a plan for an outbreak and increase hospital capacities and production of medical supplies. Testing was also faulty at first which caused a delay. However, by March legislation was passed that allowed individuals with private insurance plans, Medicare, and Medicaid to get tested with no out-of-pocket cost. Uninsured people also receive the same benefits which are funded by the National Disaster Medical System. Additionally, burden on physicians has also been lessened by giving pharmacists some of the responsibility of prescribing medications so doctors can prioritize more important cases. As telemedicine is becoming more pertinent and useful, Medicare has also waived requirements so that the eledery do not have to put themselves at risk by going to facilities in person.
Implications for Healthcare Reform
The pandemic has highlighted some of the issues in healthcare that can be improved in different areas of policy. With job losses and decreased financial resources, many individuals are either losing insurance or having decreased coverage as employers cut back on costs. Healthcare in the United States centered around fee-for-service business is contributing to the negative effects of COVID-19 on the country. When the market for services breaks down, healthcare providers who operate this business collapse as well.
The pandemic has made policy makers question whether healthcare is a vital resource that requires more secure financing than what is provided by the fee-for-service system. Even during normal times, this system results in raised prices, shortages of services such as behavioral health, and reduced service in low-income communities.
There has been extensive debate about how to reform healthcare in the United States. Several options have been proposed:
Establishing a single payer system such as Medicare for All in which the government finances all costs
Fixing existing flaws of the employee/employer private insurance system which would prevent healthcare costs from being added to a federal budget that already has a significant deficit
Introducing incremental steps towards universal healthcare such as expanding Medicaid and having the government absorb those costs, extending Affordable Care Act (ACA) coverage, or having citizens with employer plans purchase government provided insurance plans instead (public option)
With the presidential election coming up in the United States, it is more important than ever to think about these options when voting.
Conclusion
In summary:
The four models of healthcare systems in different nations are Beveridge, Bismarck, National Health Insurance, and Out-of-Pocket
The United States is a patchwork of all of these models depending on factors such as age and socioeconomic status
Countries had varied COVID-19 responses due to different healthcare systems and levels of preparedness from previous outbreaks
The United States needs to assess the effects COVID-19 has had on healthcare and strategize on how to improve it
Actions that you can take:
Learn more about your own healthcare - How is it financed? Has the pandemic affected it in any way? Do you think your plan is sustainable in emergencies such as this one?
Become more educated on the healthcare reform policies of candidates in elections
Form educated opinions on these different plans based off your own research
Evaluate how your own needs align with these plans
VOTE in the United States presidential election this November
For more about COVID-19 and its impact around the world, sign up for our newsletter here